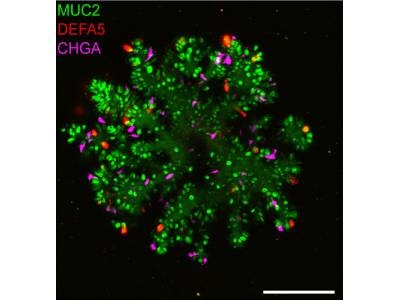
Improved small intestinal organoid with Paneth cells in red. Credit: Hubrecht Institute
Human organoids serve as excellent models for studying human biology with regard to diseases, drug reactions and more. Optimized organoid models should be as biologically similar to real human tissues as possible, which is why the absence of mature Paneth cells in human small intestinal organoids has posed a challenge for fully understanding small intestinal function and diseases such as inflammatory bowel disease (IBD). Now, researchers from the Organoid group (formerly the Clevers group) at Hubrecht Institute have developed improved human small intestinal organoids that include every cell type – including mature Paneth cells – expanding opportunities to study the functions of these cells and their role in intestinal health.
The team developed an optimized culture protocol that includes a two-step patterning-maturation protocol, which promotes the differentiation of human intestinal organoid cells toward secretory lineages and supports the expansion of organoids with extensive, crypt-like budding structures, the authors wrote. The researchers surprisingly found that Interleukin-22 (IL-22) increased the numbers and activities of Paneth cells, enabling the development of organoids that better mimic healthy small intestines. This research was published in Cell Stem Cell.
“At the moment, people believe that IL-22 can promote stem cell function,” said first author Gui-Wei He. “Our study actually showed that IL-22 does not do this, but rather stimulates the activation of Paneth cells.”
Paneth cells are important in preventing infections, as they produce antimicrobial peptides that act against harmful bacteria. A lack of active Paneth cells leads the small intestine to being more prone to infections, which is a problem in several diseases, including IBD. With the new optimized intestinal organoids available, and the discoveries about the effect of IL-22, researchers can expand the way they study small intestine biology. For example, researchers could use the organoids to alter the DNA of cells and determine how mutations – such as those occurring in diseases like IBD – will affect the function of the small intestine.
“By probing the direct effects of IL-22 on the induction of the various epithelial cell types of the human small intestinal epithelium, our study demonstrates that the optimized culture condition markedly improves ex vivo modeling of the human intestinal epithelium and significantly broadens the application of human intestinal organoids,” the authors concluded.