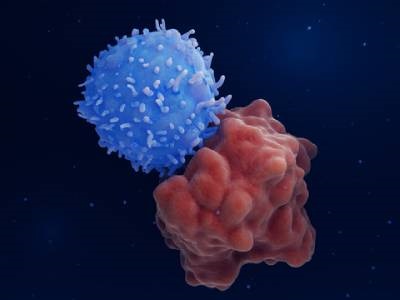
T cell transfer therapy, including CAR-T cell therapy, is a promising approach to cancer treatment that uses immune cells to fight tumors. While CAR-T cell therapies have been used to treat immune system cancers, such as leukemias and lymphomas, they have not yet been successfully used to treat solid tumors due to a number of challenges, which include the inability of T cells to easily penetrate solid tumors and to persist amidst an immune-suppressive tumor microenvironment. Combining T cell transfer therapies with cytokine therapy could help overcome these challenges, but cytokines come with their own challenges, as they can lead to toxicity and potentially fatal inflammatory syndromes when freely circulating in the body. Now, researchers from the Wyss Institute for Biologically Inspired Engineering at Harvard University, the Harvard John A. Paulson School of Engineering and Applied Sciences, and the Dana-Farber Cancer Institute have developed a new technique that anchors cytokines to T cells, reducing toxic side effects and enhancing T cells’ anti-tumor activity.
The researchers took a nanotechnology approach to conjugate the cytokines to the surface of T cells. They engineered sugar nanoparticles containing an azido group that are processed using the cells’ natural sugar metabolism, causing the nanoparticles to be incorporated into complex sugar chains on the cell surface, explained first author Yutong Liu. After the engineered sugars are incorporated, click chemistry enables modified cytokine molecules containing highly compatible DBCO groups to attach to the azido groups. This connection enables the cytokines to locally enhance T cell function while reducing the systemic side effects typically associated with cytokine therapy. The sugar nanoparticles and cytokines are added to culture media during standard T cell manufacturing processes, making the technique easy to integrate into current manufacturing pipelines, said Liu.
The team tested the cytokine-linked T cells by using them to treat mice with different types of tumors. In mice with solid melanoma tumors, they found that melanoma-specific T cells carrying the cytokine interleukin-12 (IL-12) significantly delayed tumor growth and prolonged the animals’ life spans by 50%, at non-curative doses; equal doses of melanoma-specific T cells paired with a systemic injection of IL-12 produced much weaker effects than the cytokine-linked cells. In addition, the tumors and spleens of the animals that received the cytokine-labeled T cells contained more T helper and cytotoxic T cells than the control group, according to Liu. The researchers hypothesize that the IL-12 linked T cells more effectively stimulate dendritic cells, leading to an antigen-spreading effect that aids in the destruction of solid tumors with heterogeneous cell compositions. IL-12 conjugated CAR-T cells were also used in a mouse xenograft lymphoma model, and were successful in controlling tumor development and prolonging the survival of the mice, performing better than CAR-T cells lacking IL-12. This research was published in the Proceedings of the National Academy of Sciences (PNAS).
“The straight-forward and elegant nature of [this] new approach to cancer immunotherapy offers huge potential for cancer patients,” said Wyss Founding Director Donald Ingber. “We are excited to support this effort through the Wyss Institute’s high-priority Validation Project program, which will hopefully expedite its advancement towards the clinic.”